In 2006, in the midst of a growing opioid epidemic, the FDA approved the new narcotic painkiller Opana.
It was a familiar drug.
Under the name Numorphan, it had been abused in the 1960s and 1970s
until it was removed from the market. When injected, the drug is 10
times as potent as morphine.
And now there is a familiar problem.
Known generically as oxymorphone, the FDA approved the new version of
the drug -- made by Endo Pharmaceuticals -- in 2006 as both an
immediate-release and extended-release pill. Then in December 2011, the
agency approved a new abuse-deterrent version -- but users have been
able to foil the anti-injection mechanism and have been shooting up
Opana.
In addition to overdose risk, abuse of Opana by injection has been tied to a recent outbreak of HIV in rural Indiana as well as a surge in hepatitis C infections in several Appalachian states.
It also has been associated with a blood-clotting disorder and permanent organ damage -- a problem that didn't occur with injection abuse of generics and the earlier version of the drug.
When Opana was approved, it joined more than a dozen other narcotic painkillers on the market.
"There certainly didn't seem to be a need for it," said James Roberts, MD,
a professor of emergency medicine at Drexel University College of
Medicine in Philadelphia. "There are plenty of narcotics around for pain
relief."
As Numorphan, the drug's popularity among addicts was due to its quick and sustained effect, according to the 1974 report "Drugs and Addict Lifestyle" by the National Institute on Drug Abuse.
The report said the drug -- which carried a street name of "blues"
-- was used primarily by white males and highlighted 309 Philadelphia
area addicts who were interviewed about their Numorphan abuse in 1970.
Many of the addicts said they preferred the drug over heroin.
Originally approved in 1959, FDA records indicate the pill form of
Numorphan was taken off the market in 1979 for what is described as "commercial reasons." Its intravenous and suppository formulations were allowed to remain on the market.
In an email, FDA spokesman Eric Pahon said opioids, including Opana,
are important medications for the treatment of pain, when used properly.
"The FDA is concerned about the misuse and abuse of prescription
opioids, which is a serious public health challenge, and is working in
many ways to help prescribers and patients make the best possible
choices about how to use these powerful drugs," he said. "We must
balance this effort, however, with ensuring prescribers and patients
maintain access to these medications and a variety of treatment options
are available."
Opana ER generated 756,000 prescriptions and sales of $385 million in
2013, according to data supplied by IMS Health, a drug market research
firm. Since 2009, its annual sales have ranged from $246 million to $640
million.
In an email, Endo spokesperson Heather Zoumas Lubeski said the drug
"was approved by the FDA based upon its demonstration of safety and
effectiveness in clinical trials and its successful submission of an
application for approval."
Meetings Impact Approval?
A Milwaukee Journal Sentinel/MedPage Today examination found
oxymorphone's re-appearance on the market followed a pattern identified
in past investigations, including cozy relationships between regulators
and drug company executives and the use of questionable clinical
testing methods allowed by the FDA.
Endo was a frequent participant at meetings of an organization funded
by pain drug companies that brought together pharmaceutical executives
and federal regulators during the 2000s, records show.
The group, known as IMMPACT, was the subject of a 2013 Journal Sentinel/MedPage Today investigation.
The story highlighted how federal health industry officials, members
of academia, and executives of companies that make pain drugs held
private meetings at expensive hotels at least once a year beginning in
2002, according to emails obtained through a public records request.
Each year, a handful of drug companies paid up to $35,000 each to
send a representative to the meetings where they could discuss clinical
trial design with FDA officials.
The arrangement was criticized as appearing to be pay-for-play
connection between regulators and companies anxious to get products onto
the multibillion-dollar-a-year pain market.
In 2014, two U.S. senators wrote to the medical school dean at the University of Rochester demanding financial records related to the IMMPACT meetings. A researcher at the school was a co-founder of the group.
Sen. Joe Manchin (D-W.Va.) and Sen. David Vitter (R-La.) wrote that
they were "deeply troubled by allegations that the FDA gave
manufacturers of prescription drugs the opportunity to pay thousands of
dollars to the University of Rochester Medical Center for the privilege
to attend private meetings with FDA officials."
FDA spokesman Pahon said it is misleading to imply that the IMMPACT
meetings were private meetings between FDA officials and members of
industry.
Though the meetings were invitation-only, he said, they were attended
by a variety of government officials, academics, and pain advocates.
"These were large scientific meetings at which the outside experts
almost always outnumbered the attending companies," he said. "We are not
aware of any separate, private meetings between FDA and pharmaceutical
companies during or as a result of IMMPACT meetings."
He said the meetings had no bearing on the approval of Opana and did
not include the discussion of any particular product or the standards
for FDA approval of pain products.
Stacking the Deck?
The IMMPACT meetings helped develop a new approach to winning approval of drugs known as enriched enrollment.
The approach allows drugs companies to weed out people who don't
respond well to a drug or who can't tolerate taking it before an actual
clinical trial for the drug begins.
Independent doctors say that approach makes it much more likely a
drug will be found effective and possibly win FDA approval. It's also
cheaper for drug companies to conduct such trials.
Critics say the approach essentially stacks the deck in favor of the
drug. More importantly, experts say, drugs tested that way are not
likely to reflect what will happen when a medication gets on the market
and is prescribed for large numbers of people.
When Endo tried to get Opana approved in 2003, the FDA said the drug
didn't appear effective enough in clinical trials. It also raised safety
concerns after several postoperative pain patients overdosed on the
drug and had to be revived with naloxone.
So Endo conducted new clinical trials using enriched enrollment.
In those trials, only the patients who initially responded to the
drug were entered into a randomized, controlled trial, where they were
given either Opana or a placebo. The idea is that the drug's effects can
be clearly demonstrated in comparison with placebo because it is
already known to work for all of the patients.
The results of those trials helped get the drug approved by the FDA
in 2006. But the FDA's own medical review of the drug acknowledged that,
given the enriched study design, "one could argue that the results may
not be generalizable to the wider chronic pain population."
"The FDA should be in the business of requiring high-quality evidence and not short-cut evidence," said Lewis Nelson, MD,
a medical toxicologist at NYU Langone Medical Center. "Unfortunately,
they're under pressure to make pharmaceuticals available to the general
public."
Nelson said the enriched trials "find the people who are most likely to respond to a drug and not suffer from side effects."
"I don't think enriched enrollment studies are truly valid," he added.
FDA spokesman Pahon said companies use a variety of strategies to
select those in the general population in which the effect of a drug can
be more readily shown.
He would not say whether the FDA encouraged Endo to use enriched enrollment for Opana.
"You'll need to FOIA [apply under the Freedom of Information Act to see] those pre-approval meeting minutes," he said.
Opana is not the only opioid approved using enriched enrollment. In 2013, drugmaker Zogenix used the strategy to win approval for Zohydro, a high-dose, hydrocodone-only drug that was originally approved without any abuse-deterrent mechanisms.
| Medpage Today
Sunday, May 10, 2015
Sunday, April 26, 2015
Radically Rethinking Medical Education : Shots
Katherine Streeter for NPR
"Why do I need to know this stuff?" medical students ask me.
"How many times have you used the Krebs Cycle lately?" senior doctors jokingly reminisce.
For decades, first-year medical students have had to cram the details of the Krebs cycle into their heads. Now the biomedical model of educating doctors, based largely on a century-old document called The Flexner Report, is coming under fire.
From one end, our long-standing medical education model is attacked as out of tune with the information age. By some estimates, our entire body of medical knowledge doubles every three or four years.
Critics say med students can't possibly master so much
information, which quickly becomes outdated anyway. Instead, the new
theory goes, students should be taught and evaluated on their ability to
find, assess and synthesize knowledge. And they should be educated in teams to help prepare them for what goes on in the real world.
From
another angle, critics of the Flexner model correctly point out that
Flexner himself, an educational theorist with no medical training, was
silent on issues such as poverty, housing, nutrition and other factors
that we now call the social determinants of health.
We now know these factors collectively affect our overall health more than even the $3 trillion health care industry.
Many
times I've seen patients and found the tools I was trained to use
aren't nearly enough to provide help. No physical exam or X-ray can find
a homeless person a bed. No lab test or medication can provide a
laid-off worker with job training or education.
It took more
than a decade for me to learn to ask patients about hunger. I found out
that many of the people I've cared for suffer from food insecurity – not
knowing where their next meal will come from.
"But what can I do about those problems?" my students ask. "Isn't that just social work?"
The answer may surprise you.
In my role as a medical educator, I attended the Beyond Flexner conference in Albuquerque, N.M., in early April. The main theme of the meeting, sponsored by the W.K. Kellogg Foundation and others, was this question: "What is the social mission of medical education?"
The conference came about as an outgrowth of a 2010 paper that ranked medical schools by their social commitment rather than their research dollars or U.S. News and World Report
scores. It began as something of a shot across the bow to organized
medicine, challenging orthodoxy, such as making students memorize the
Krebs cycle.
Over the years since then, more research has shed light on the economic and health impact of social determinants. The media has caught on to this as well.
Nearly
400 medical educators, activists, policymakers and students turned up
to share ideas, hash out strategy and plan a road map for changing
medical education.
Our hosts from the University of New Mexico
demonstrated that medical schools that are serious about community
engagement build strong partnerships that take social determinants into
account. We heard how community health workers and a re-imagination of
the agricultural extension model for health education are improving the health of New Mexicans.
To
me, the most surprising aspect of the meeting was just how many medical
schools are now getting serious about the importance of social
determinants.
Many of the sessions at the conference explored
obstacles that stand in the way of a culture change in medical
education. At the top of the list: How to deal with a payment system
that still prioritizes the quantity of medical care over quality? A decision
by Medicare earlier this year to base a large proportion of future
payments on quality and value has convinced many of us that the health
system is on the path of change.
I left the conference with new
ideas and fresh energy. I also was left wondering what will replace the
Krebs cycle in the medical education pantheon.
My bet? It will
be a team of students finding ways to break the vicious cycle of
poverty that contributes to so much suffering, illness and early loss of
life.
John Henning Schumann is a writer and doctor in
Tulsa, Okla. He was recently named interim president of the University
of Oklahoma, Tulsa. He also hosts Public Radio Tulsa's Medical Matters. He's on Twitter: @GlassHospital
: NPR
Friday, April 3, 2015
Safety Communications > Olympus Validates New Reprocessing Instructions for Model TJF-Q180V Duodenoscopes
Medical Specialties: Gastroenterology, Infection Control
Device: Olympus Duodenoscope model TJF-Q180V
Olympus
has issued new, validated manual reprocessing instructions for the
TJF-Q180V duodenoscope to replace those provided in the original
labeling. The FDA has reviewed these new reprocessing instructions and
the validation data as part of its ongoing review of the 510(k), and
recommends that any facilities that are using Olympus’ TJF-Q180V
duodenoscope train staff on the new instructions and implement them as
soon as possible.
Summary of Problem and Scope:
As noted in FDA’s February 2015 Safety Communication,
the complex design of ERCP endoscopes (also called duodenoscopes) may
impede effective reprocessing. Reprocessing is a detailed, multistep
process to clean and disinfect or sterilize reusable devices. Recent
medical publications and adverse event reports associate
multidrug-resistant bacterial infections in patients who have undergone
ERCP with reprocessed duodenoscopes, even when manufacturer reprocessing
instructions are followed correctly. FDA has been working with
duodenoscope manufacturers as they modify and validate their
reprocessing instructions to further enhance the safety margin of their
devices and show with a high degree of assurance that their reprocessing
instructions, when followed correctly, effectively clean and disinfect
the duodenoscopes.
In September 2014, Olympus initiated testing to
validate new reprocessing instructions. The cleaning validation reports
were provided to FDA in October 2014. While FDA found Olympus’ cleaning
validation data acceptable, initial high level disinfection reports did
not demonstrate an adequate safety margin, and so Olympus conducted
additional testing. At the end of February 2015, Olympus submitted new
high level disinfection validation data to FDA. The agency has reviewed
this data and believes that, when followed, the new, validated
reprocessing instructions for the Olympus TJF-Q180V duodenoscope are
robust, and demonstrate consistent and reliable cleaning and high-level
disinfection. At FDA’s request, Olympus has issued the new, validated
instructions for reprocessing the TJF-Q180V duodenoscope.
To
validate reprocessing instructions for duodenoscopes, manufacturers
should soil their device with bacteria to simulate use in a procedure
and then demonstrate that the device can be adequately disinfected
through a sufficient reduction in microbes when the reprocessing
instructions are correctly followed. To support high level disinfection
of duodenoscopes, the disinfectant should result in a six-log reduction
in the number of microbes at each of several locations on the scope –
that is a one million-fold reduction; or a reduction of 99.9999%.
The
FDA is closely monitoring the possible association between reprocessed
duodenoscopes and the transmission of infectious agents, including
multidrug-resistant bacterial infections caused by Carbapenem-Resistant
Enterobacteriaceae (CRE) such as Klebsiella species and Escherichia
coli. If not properly reprocessed, residual body fluids and organic
debris may remain in microscopic crevices of the device following an
attempted cleaning and high level disinfection. If these residual fluids
contain microbial contamination, subsequent patients may be exposed to
serious infections. The FDA’s investigation into the possible
association between inadequately reprocessed duodenoscopes and patient
infections, including the agency’s recommendations for health care
facilities, is more fully discussed in its February 2015 Safety Communication.
Olympus sent letters dated March 26, 2015
to health care facilities and other users of the TJF-Q180V outlining
the new, validated reprocessing instructions, and will soon be
distributing revised user manuals.
Please note the key changes to the reprocessing procedure for Olympus’ TJF-Q180V duodenoscope:
Precleaning:
recommendations are based on currently available information. If new,
important information becomes available, FDA will update its
recommendations.
As noted inFDA’s Updated Information for Healthcare Providers Regarding Duodenoscopes
issued March 4, 2015, Olympus has a pending 510(k) application for its
TJF-Q180V duodenoscope and the company continues to market its device
while its application is under review. The removal of its device from
the market could lead to an insufficient number of available
duodenoscopes to meet the clinical demand in the United State of
approximately 500,000 procedures per year.
FDA Activities:
The
FDA is actively engaged with other government agencies, including
Centers for Disease Control and Prevention (CDC), and the manufacturers
of duodenoscopes used in the United States to identify the causes and
risk factors for transmission of infectious agents and develop solutions
to further increase the safety margin of reprocessed devices and
minimize patient exposure to infectious agents.
The agency will convene a public Advisory Committee Meeting
on May 14th and 15th, 2015 to seek expert scientific and clinical
opinion related to reprocessing of duodenoscopes and other endoscopes,
as well as use of automated endoscope reprocessors for duodenoscope
reprocessing, based on available scientific information. The committee
will make recommendations on: (1) The effectiveness of cleaning, high
level disinfection, and sterilization methods; (2) the amount and type
of premarket validation data and information needed to support labeling
claims and technical instructions; (3) the appropriate use of other risk
mitigations, such as surveillance cultures; (4) best practices and
guidelines for reprocessing duodenoscopes and endoscopes at user
facilities to minimize the transmission of infections; and (5)
recommended approaches for ensuring patient safety during ERCP
procedures, including a discussion of appropriate patient selection.
Recommendations on these issues will assist FDA in minimizing patient
exposure to infectious agents that may result from reprocessed
duodenoscopes and endoscopes.
The FDA is also working closely with
the manufacturers of reusable medical devices such as duodenoscopes to
ensure that their reprocessing instructions are adequate to clean and
disinfect the devices. The FDA continues to actively monitor this
situation and will provide updates as appropriate.
Reporting Problems to the FDA:
Device manufacturers and user facilities must comply with the applicable Medical Device Reporting (MDR) regulations.
Health care personnel employed by facilities that are subject to the FDA's user facility reporting requirements should follow the reporting procedures established by their facilities.
Prompt
reporting of adverse events can help the FDA identify and better
understand the risks associated with medical devices. Health care
providers should submit voluntary reports of the transmission of an
infection due to an inadequately cleaned duodenoscope to the agency via
the Medical Device Reporting (MDR) process.
If
a health care provider suspects bacterial contamination—either because
of an increase in infections after ERCP, or because of the results of
bacterial surveillance culturing of duodenoscopes—we encourage the
health care provider to file a voluntary report through MedWatch, the FDA Safety Information and Adverse Event Reporting program.
Model TJF-Q180V Duodenoscopes
Device: Olympus Duodenoscope model TJF-Q180V
Olympus
has issued new, validated manual reprocessing instructions for the
TJF-Q180V duodenoscope to replace those provided in the original
labeling. The FDA has reviewed these new reprocessing instructions and
the validation data as part of its ongoing review of the 510(k), and
recommends that any facilities that are using Olympus’ TJF-Q180V
duodenoscope train staff on the new instructions and implement them as
soon as possible.
Summary of Problem and Scope:
As noted in FDA’s February 2015 Safety Communication,
the complex design of ERCP endoscopes (also called duodenoscopes) may
impede effective reprocessing. Reprocessing is a detailed, multistep
process to clean and disinfect or sterilize reusable devices. Recent
medical publications and adverse event reports associate
multidrug-resistant bacterial infections in patients who have undergone
ERCP with reprocessed duodenoscopes, even when manufacturer reprocessing
instructions are followed correctly. FDA has been working with
duodenoscope manufacturers as they modify and validate their
reprocessing instructions to further enhance the safety margin of their
devices and show with a high degree of assurance that their reprocessing
instructions, when followed correctly, effectively clean and disinfect
the duodenoscopes.
In September 2014, Olympus initiated testing to
validate new reprocessing instructions. The cleaning validation reports
were provided to FDA in October 2014. While FDA found Olympus’ cleaning
validation data acceptable, initial high level disinfection reports did
not demonstrate an adequate safety margin, and so Olympus conducted
additional testing. At the end of February 2015, Olympus submitted new
high level disinfection validation data to FDA. The agency has reviewed
this data and believes that, when followed, the new, validated
reprocessing instructions for the Olympus TJF-Q180V duodenoscope are
robust, and demonstrate consistent and reliable cleaning and high-level
disinfection. At FDA’s request, Olympus has issued the new, validated
instructions for reprocessing the TJF-Q180V duodenoscope.
To
validate reprocessing instructions for duodenoscopes, manufacturers
should soil their device with bacteria to simulate use in a procedure
and then demonstrate that the device can be adequately disinfected
through a sufficient reduction in microbes when the reprocessing
instructions are correctly followed. To support high level disinfection
of duodenoscopes, the disinfectant should result in a six-log reduction
in the number of microbes at each of several locations on the scope –
that is a one million-fold reduction; or a reduction of 99.9999%.
The
FDA is closely monitoring the possible association between reprocessed
duodenoscopes and the transmission of infectious agents, including
multidrug-resistant bacterial infections caused by Carbapenem-Resistant
Enterobacteriaceae (CRE) such as Klebsiella species and Escherichia
coli. If not properly reprocessed, residual body fluids and organic
debris may remain in microscopic crevices of the device following an
attempted cleaning and high level disinfection. If these residual fluids
contain microbial contamination, subsequent patients may be exposed to
serious infections. The FDA’s investigation into the possible
association between inadequately reprocessed duodenoscopes and patient
infections, including the agency’s recommendations for health care
facilities, is more fully discussed in its February 2015 Safety Communication.
Olympus sent letters dated March 26, 2015
to health care facilities and other users of the TJF-Q180V outlining
the new, validated reprocessing instructions, and will soon be
distributing revised user manuals.
Please note the key changes to the reprocessing procedure for Olympus’ TJF-Q180V duodenoscope:
Precleaning:
- During immersion, raise and lower the elevator three times
- Additional brushing of the forceps elevator recess area
- The
revised cleaning procedure requires brushing of the forceps elevator
recess with two different-sized brushes. In addition to the brush that
is currently used to clean the elevator recess area, the MAJ-1888 brush
(or MAJ-1888 equivalent) will be provided for further cleaning of this
area. Olympus anticipates shipping the MAJ-1888 brushes to facilities no
later than May 8, 2015.
- The
- Additional flushing of forceps elevator recess area
- Additional raising/lowering the forceps elevator
- Additional manual flushing steps and increased flushing volume of each endoscope channel, as well as the elevator recess area
- Additional raising/lowering the forceps elevator
- Implement
the new manual cleaning and high level disinfection procedures for the
Olympus TJF-Q180V duodenoscope in accordance with the manufacturer’s
reprocessing instructions- Implement the new TJF-Q180V high level
disinfection procedure immediately. The high level disinfection
procedure does not require additional equipment for implementation. - Implement
the new TJF-Q180V manual cleaning procedure as soon as possible. It
involves the use of a new, smaller bristle cleaning brush (model
MAJ-1888) which Olympus anticipates shipping to facilities no later than
May 8, 2015. Continue using the existing cleaning procedure for manual
cleaning of the TJF-Q180V until the new brush is available.
- Implement the new TJF-Q180V high level
- Train appropriate staff on Olympus’ new reprocessing instructions and implement them as soon as possible.
- Contact
Olympus directly with specific questions and concerns or to schedule a
site visit with their Endoscopy Support Specialists:- Technical Assistance Center (TAC), 1-800-848-9024, option 1 Monday - Friday between 7AM EST - 8 PM EST.
recommendations are based on currently available information. If new,
important information becomes available, FDA will update its
recommendations.
As noted inFDA’s Updated Information for Healthcare Providers Regarding Duodenoscopes
issued March 4, 2015, Olympus has a pending 510(k) application for its
TJF-Q180V duodenoscope and the company continues to market its device
while its application is under review. The removal of its device from
the market could lead to an insufficient number of available
duodenoscopes to meet the clinical demand in the United State of
approximately 500,000 procedures per year.
FDA Activities:
The
FDA is actively engaged with other government agencies, including
Centers for Disease Control and Prevention (CDC), and the manufacturers
of duodenoscopes used in the United States to identify the causes and
risk factors for transmission of infectious agents and develop solutions
to further increase the safety margin of reprocessed devices and
minimize patient exposure to infectious agents.
The agency will convene a public Advisory Committee Meeting
on May 14th and 15th, 2015 to seek expert scientific and clinical
opinion related to reprocessing of duodenoscopes and other endoscopes,
as well as use of automated endoscope reprocessors for duodenoscope
reprocessing, based on available scientific information. The committee
will make recommendations on: (1) The effectiveness of cleaning, high
level disinfection, and sterilization methods; (2) the amount and type
of premarket validation data and information needed to support labeling
claims and technical instructions; (3) the appropriate use of other risk
mitigations, such as surveillance cultures; (4) best practices and
guidelines for reprocessing duodenoscopes and endoscopes at user
facilities to minimize the transmission of infections; and (5)
recommended approaches for ensuring patient safety during ERCP
procedures, including a discussion of appropriate patient selection.
Recommendations on these issues will assist FDA in minimizing patient
exposure to infectious agents that may result from reprocessed
duodenoscopes and endoscopes.
The FDA is also working closely with
the manufacturers of reusable medical devices such as duodenoscopes to
ensure that their reprocessing instructions are adequate to clean and
disinfect the devices. The FDA continues to actively monitor this
situation and will provide updates as appropriate.
Reporting Problems to the FDA:
Device manufacturers and user facilities must comply with the applicable Medical Device Reporting (MDR) regulations.
Health care personnel employed by facilities that are subject to the FDA's user facility reporting requirements should follow the reporting procedures established by their facilities.
Prompt
reporting of adverse events can help the FDA identify and better
understand the risks associated with medical devices. Health care
providers should submit voluntary reports of the transmission of an
infection due to an inadequately cleaned duodenoscope to the agency via
the Medical Device Reporting (MDR) process.
If
a health care provider suspects bacterial contamination—either because
of an increase in infections after ERCP, or because of the results of
bacterial surveillance culturing of duodenoscopes—we encourage the
health care provider to file a voluntary report through MedWatch, the FDA Safety Information and Adverse Event Reporting program.
Model TJF-Q180V Duodenoscopes
GastroBreak: White House War on 'Superbugs,' CMS Hep C $$
The latest news and research in gastroenterology.
The White House published an extensive plan to slow the emergence and spread of antibiotic-resistant bacteria, including carbapenem-resistant Enterobacteriaceae (CRE), methicillin-resistant Staphylococcus aureus (MRSA), and Clostridium difficile.Olympus has issued new disinfecting instructions for its duodenoscopes, which are unapproved by the FDA and have been linked to carbapenem-resistant Enterobacteriaceae (CRE) infections at UCLA Medical Center.
Medicare spent $4.5 billion in 2014 on hepatitis C drugs, a 15-fold
increase compared with 2013's spending on earlier generation
medications, reported ProPublica.
Nearly two-thirds of patients with colorectal cancer have survival
rates of greater than 5 years, due to improvements in early detection
and treatment, according to a CDC report.
But one-third of adults are still not getting the recommended screening for colon cancer. One gastroenterologist explains how to decrease that number.
Patients with inflammatory bowel disease who are on immunosuppressive
therapy have a less robust response to routine vaccinations, reported
researchers in Digestive Diseases and Sciences.
Three alcoholic drinks per day can cause liver cancer, while coffee may have a protective effect, according to a report published by the Continuous Update Project.
| Medpage Today
Wednesday, March 4, 2015
Clinical Practice Guidelines for the Medical Management of Non-Hospitalized Ulcerative Colitis: The Toronto Consensus - Gastroenterology
Background & Aims
The medical management of ulcerativecolitis (UC) has improved through the development of new therapies and
novel approaches that optimize existing drugs. Previous Canadian
consensus guidelines addressed the management of severe UC in the
hospitalized patient. We now present consensus guidelines for the
treatment of ambulatory patients with mild-to-severe active UC.
Methods
Asystematic literature search identified studies on the management of
UC. The quality of evidence and strength of recommendations were rated
according to the Grading of Recommendation Assessment, Development, and
Evaluation (GRADE) approach. Statements were developed through an
iterative online platform, then finalized and voted on by a working
group of specialists.
Results
The participants concludedthat the goal of therapy is complete remission defined as both
symptomatic and endoscopic remission without corticosteroids. The
consensus includes 34 statements focused on five main drug classes,
5-aminosalicylate (ASA), corticosteroids, immunosuppressants, anti-tumor
necrosis factor-alpha (TNF) therapies, and other therapies. Oral and
rectal 5-ASAs are recommended first-line therapy for mild-to-moderate
UC, with corticosteroid therapy for those who fail to achieve remission.
Patients with moderate-to-severe UC, should undergo a course of oral
corticosteroids, with transition to 5-ASA, thiopurines, anti-TNF therapy
(with or without thiopurines or methotrexate), or vedolizumab
maintenance therapy in those who successfully achieve symptomatic
remission. For patients with corticosteroid-resistant/dependent UC,
anti-TNF therapies or vedolizumab are recommended. Timely assessments of
response and remission are critical to ensuring optimal outcomes.
Conclusions
Optimalmanagement of UC requires careful patient assessment, evidence-based
use of existing therapies, and thorough assessment to define treatment
success.
- Gastroenterology
Sunday, February 22, 2015
Smartphones, tablets can do damage to overall health in unexpected ways
Despite the many benefits of having information at your fingertips, smartphones and tablets can do damage to your body and
overall health in unexpected ways.
 You may not realize it, but all that time spent with your head down
You may not realize it, but all that time spent with your head down
checking email and texting may be creating more than a social gap — you
may also be harming your spine. Research suggests that spinal pressure
actually doubles with each inch you bend your head down.
Smartphone users spend an average of two to four hours per day
hunched over, says Kenneth Hansraj, chief of spine surgery at New York
Spine Surgery & Rehabilitation Medicine, in his recent report for
Surgical Technology International. As a result, back and neck pain have
increased among users of electronic gadgets, and the effects may linger
for years.
"Poor posture is easy to spot in the hunched over forms of older
adults who have carried bad habits for a lifetime," said Stephen
Gubernick, Doctor of Chiropractic at The Joint Chiropractic. "However,
few people realize that there are health implications that make good
posture essential for healthy living at any age."
Dr. Gubernick explained that a misalignment of your spine can affect
your overall health and well-being. Your spine protects your nervous
system, which controls and coordinates all the different functions of
your body. Any disruption in nerve communication to your organs and
tissues may result in abnormal function. "There are countless benefits
from simply improving the alignment of the spine," he added.
Poor posture negatively impacts your muscles and ligaments, as well
as your spine, which can lead to a host of health problems ranging from
neck and back pain to gastrointestinal problems and even hyperkyphosis —
a condition in which the spine curvature is significantly exaggerated,
with increased risk of pulmonary and arterial health problems.
When posture or other factors cause a misalignment, a spinal
adjustment is one way to help restore normal nerve function and
communication, thereby allowing your body to work normally and
naturally.
In addition to recommending exercises that strengthen your core
postural muscles in an effort to sustain and improve posture, a
chiropractor can also assist you with identifying proper posture
techniques to use during daily activities that help reduce the risk of
injury.
Why Posture Matters
There are many benefits to practicing good posture. According to the
American Chiropractic Association, keeping your spine aligned properly:
Ditching your smartphone probably isn't a practical solution for
improving your posture, so instead work to keep your posture in check
with these tips:
overall health in unexpected ways.
 You may not realize it, but all that time spent with your head down
You may not realize it, but all that time spent with your head down checking email and texting may be creating more than a social gap — you
may also be harming your spine. Research suggests that spinal pressure
actually doubles with each inch you bend your head down.
Smartphone users spend an average of two to four hours per day
hunched over, says Kenneth Hansraj, chief of spine surgery at New York
Spine Surgery & Rehabilitation Medicine, in his recent report for
Surgical Technology International. As a result, back and neck pain have
increased among users of electronic gadgets, and the effects may linger
for years.
"Poor posture is easy to spot in the hunched over forms of older
adults who have carried bad habits for a lifetime," said Stephen
Gubernick, Doctor of Chiropractic at The Joint Chiropractic. "However,
few people realize that there are health implications that make good
posture essential for healthy living at any age."
Dr. Gubernick explained that a misalignment of your spine can affect
your overall health and well-being. Your spine protects your nervous
system, which controls and coordinates all the different functions of
your body. Any disruption in nerve communication to your organs and
tissues may result in abnormal function. "There are countless benefits
from simply improving the alignment of the spine," he added.
Poor posture negatively impacts your muscles and ligaments, as well
as your spine, which can lead to a host of health problems ranging from
neck and back pain to gastrointestinal problems and even hyperkyphosis —
a condition in which the spine curvature is significantly exaggerated,
with increased risk of pulmonary and arterial health problems.
When posture or other factors cause a misalignment, a spinal
adjustment is one way to help restore normal nerve function and
communication, thereby allowing your body to work normally and
naturally.
In addition to recommending exercises that strengthen your core
postural muscles in an effort to sustain and improve posture, a
chiropractor can also assist you with identifying proper posture
techniques to use during daily activities that help reduce the risk of
injury.
Why Posture Matters
There are many benefits to practicing good posture. According to the
American Chiropractic Association, keeping your spine aligned properly:
- Ensures bones and joints are correctly aligned. This helps the
muscles to be used properly, diminishing the abnormal wear which can
cause degenerative arthritis and joint pain. - Places less stress on the ligaments which link the spinal joints, decreasing the chance of injury.
- Creates efficiency within the muscle groups, helping the body use less energy and avoid fatigue.
- Reduces the likelihood of back and muscular pain, overuse disorders and muscle strain.
Ditching your smartphone probably isn't a practical solution for
improving your posture, so instead work to keep your posture in check
with these tips:
- To protect your posture while using your phone and other electronic
devices, avoid angling your head down for prolonged periods. Raise the
device closer to eye level, or use a stand to prop the screen. - Treat back and neck pain, which may signal a posture problem or
worsen poor posture habits, with regular chiropractic adjustments to
keep your body balanced and flexible. - When sitting, avoid crossing your legs and keep your knees at or
below hip level. Use a back pillow to support your lower and middle
back. Relax your shoulders and avoid sitting in the same position for
extended periods of time. - While standing, keep your feet shoulder width apart and your knees
slightly bent. Stand straight with your shoulders pulled back and your
stomach tucked in.
Source:
Family Features Editorial Syndicate
Friday, February 20, 2015
CRE outbreak: You're due to go in for a procedure. Should you be worried? - CNN.com
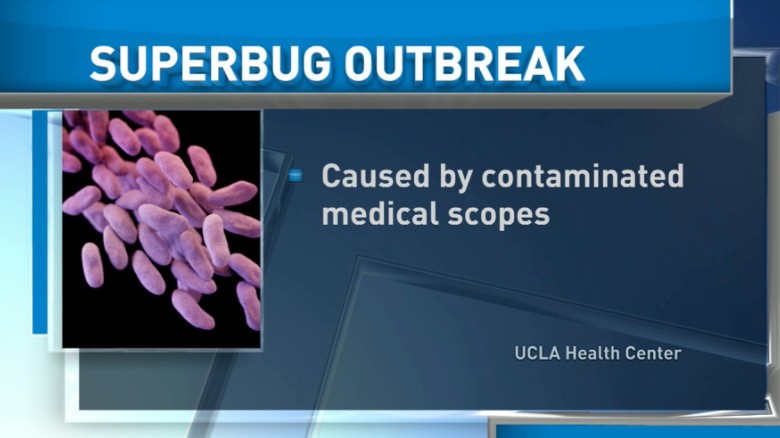
UCLA narrows cause of superbug infection to 2 tools 01:15
(CNN)You're due to go in for a medical procedure. But after what happened at a UCLA hospital, you're a little apprehensive.
Twopatients died at the Ronald Reagan UCLA Medical Center in a superbug
CRE outbreak, caused by two medical scopes that still carried the
bacteria even after they were disinfected.
In addition to the two
victims, seven hospital patients were infected with the deadly superbug
between October and January. The medical center has contacted 179
others who had endoscopic procedures between October and January and is
offering them home tests to screen for the bacteria.
The superbug, carbapenem-resistant Enterobacteriaceae, or CRE, can kill up to half the patients who contract them, the Centers for Disease Control and Prevention says.
So, should you cancel your procedure?
Here's what you need to know:
1. What type of equipment caused these horrible infections?
They're called duodenoscopes.
The
UCLA hospital was using a duodenoscope made by Olympus Corp. of the
Americas, but the Food and Drug Administration is also reviewing data
from the two other U.S. companies that make the devices, Fujifilm USA
and Pentax Medical.
Duodenoscopes are most commonly used for
procedures on the gallbladder, pancreatic ducts, and the bile ducts,
which are a series of thin tubes that reach from the liver to the small
intestine.
2. I'm scheduled to get a colonoscopy soon. Should I be worried?
No. Duodenoscopes are not used for colonoscopies.
3. How common are these infections, and why do they happen?
More
than half a million duodenoscope procedures are done every year in the
United States, and there have been fewer than 100 known cases of
transmission of the CRE bacteria, according to the American Society for Gastrointestinal Endoscopy.
The problem is this: A part of the scope called "the elevator" can be tough to clean because it has many small moving parts.
According to the FDA, the cleaning instructions that come with duodenoscopes say to brush the elevator area -- but that might not be enough.
"The
moving parts of the elevator mechanism contain microscopic crevices
that may not be reached with a brush," the FDA said Thursday. "Residual
body fluids and organic debris may remain in these crevices after
cleaning and disinfection. If these fluids contain microbial
contamination, subsequent patients may be exposed to serious
infections."
4. Yech. I'm supposed to have a procedure with a duodenoscope. Should I cancel it?
No.
A procedure with a duodenoscope can be lifesaving. It can remove
gallstones, for example, or insert a stent into a blocked bile duct. If
you need it, you need it.
5. OK. My doctor says I need it. So how do I make sure I'm safe?
Remind your doctor that following the manufacturer's cleaning instructions on a duodenoscope might not be enough.
Show your doctor this advisory from the FDA
that recommends additional cleaning practices, including meticulously
cleaning the elevator mechanism by hand. Many hospitals already do this.
Also, show your doctor this article from the Centers for Disease Control:
A hospital in Illinois put a stop to duodenoscope infections by using a
technique called gas sterilization. Other hospitals have started
testing their scopes for bacteria and only using them when the results
come back negative.
- CNN.com
Thursday, February 19, 2015
Why Your Doctor Might Not Be the Best Nutritional Resource

and rightfully so. While you should trust their advice on certain
matters, it's also important to understand the boundaries of their
training, and when you should seek outside help.
I grew up obese despite the fact that both my parents were medical
doctors, and fit ones at that. The few conversations we had about my
weight were essentially lectures on moderation (or simply "eat less, move more").
I always figured the lack of intervention was probably because they
assumed I'd grow out of the chub. Besides, it can't be easy for someone
to dual as parent and diet coach.
Fast forward two decades, and the story is completely different. My
father is now overweight, pops countless (medical) pills for breakfast.
He doesn't know the first thing about losing weight, nor does he care to
learn. Contrastingly, my mother is in great shape, thanks to becoming
an avid consumer of fitness information following my own transformation.
Looking back, I now know that their silence wasn't because they were
hesitant or unwilling to help me lose weight. It was because they had no
clue how to help me lose weight.
My parents are just n=2, but in my coaching experience, many clients
have reported a similar gap in their own GP's knowledge. Sure, their
doctor can tell them when to lose weight, but dispense poor advice to
help them achieve it. This is unsurprising.
What Doctors Know: Disease vs. Health
undergraduate program, four years in medical school, and at least three
years in residency (depending on chosen area of expertise). Basically,
doctors learn a whole lot about a whole bunch of stuff, for a long time.
But in all those years, and all those textbooks, very little of that is
about nutrition—the biggest factor in weight loss, and debatably one of the most important factors for overall health.
Of the 40,000 hours that doctors spend on training, typically only 19 of those are devoted to studying nutrition. According to the Chicago Tribune, this number is steadily decreasing:
On average, doctors receive 19 hours of total nutrition education inAs such, it shouldn't be surprising that a study from The Journal of the American College of Nutrition
medical school; in 2004 the average was 22.3 hours, according to the
study, conducted as part of the Nutrition in Medicine project at UNC. In
2009, 27 percent of the schools met the minimum standard of nutrition
training, compared with 38 percent in 2004.
shows that only 14% of internal medicine interns feel they can
adequately talk to their patients about nutrition, while 94% feel it's
their responsibility to do so. Yet, if Dr. Oz's popularity ratings are
any indication, society still considers doctors to be weight loss
authorities.
To be clear, this is a systematic failing of the medical educational
system, and not the fault of our doctors. Between seeing patients and fixing them—something that they are
incredibly knowledgeable about—there's not a lot of time to make up for
their educational shortcomings. Still, it seems silly to look to medicine to reduce incidence of disease, when dietary intervention may have prevented some of these in the first place.
The Problem with Defaulting to Doctors for Nutritional Advice

which is in no way helped by the apparent paralysis of relevant
regulatory parties. Case in point: despite decades of outcry from the
scientific community, the FDA is only now relaxing its message on the dangers of dietary cholesterol.
With conflicting information abound, people deal with confusion in different ways. Some are autodidacts,
or self-learners, who read voraciously until they can navigate through
the noise. Most people, however, naturally default to someone they trust
to tell them what to do.
Human beings are subject to something called bounded rationality—the
idea that, in the face of complexity, humans sacrifice calculating the
purely rational choice by making mental shortcuts. For most people,
doctors are the gatekeepers of health information. They know doctors are
educated in their profession, and generally trustworthy. Therefore, it
seemingly follows that a doctor's health advice must be reliable.
The problem is that too many people think that "curing disease" is
the same thing as "preventing disease." In reality, these are two
completely different areas of expertise. As my friend Dr. Joseph
Lightfoot once told me: "In medical school, I learned about disease, but
I did not learn about health."
In spite of this, it's hard to imagine a doctor's typical nutritional
recommendations could be harmful, after all how dangerous could an
abundance of cruciferous vegetables be?However, the utility of their
advice is undermined by one of medicine's most basic tenets: "First do
no harm." In other words, they must make sure that any treatment does
not make a patient's situation worse. For nutrition, this often
translates into stock-standard dietary advice.
For example, let's say a doctor is faced with the choice of giving a
recommendation that's in line with the status quo, such as limiting
sodium, or going against the grain by saying that you shouldn't worry
about salt intake. In the doctor's eyes, which is more likely to "do no
harm?" Most doctors would avoid the controversy and just tell their
patient to limit their salt intake, because that's what everyone has
always said. Their assumption is that this advice "does no harm."
The problem is that it does do harm. It increases their
patient's chances of failure, thereby precluding them from the benefits
of maintaining a healthy weight and an enjoyable lifestyle. Quite
simply, research shows that the best diet is one you can stick to. By creating false restrictions
and limiting choice, you state that there is only one path for success
(the doctor's)—a low sodium, low saturated fat, low cholesterol,
alcohol-free one—when in reality there are many.
According to obesity specialist and frequent Lifehacker contributor Dr. Spencer Nadolsky:
Unless trained through ABOM (American Board of Obesity Medicine),
ABPNS (American Board of Physician Nutrition Specialists ), or similar
training/experience, the typical doctor isn't as well equipped to help
with dietary guidance. This doesn't mean the doctor is bad, it just
means it wasn't in their training.
How to Find a Doctor That Can Help You

another frequent Vitals contributor. In fact, because of their
multi-domain expertise, these doctors have unique insights around
preventative health and disease that few others possess. The danger, however, is that assuming that all medical doctors have this same expertise.
Here's how to find out if your doctor can help you with your own nutrition and fitness endeavors:
- Research the latest evidence on topics such as saturated fat, protein intake, and dietary cholesterol. Examine.com's FAQ
is a good place to start. Ask your doctor questions about these topics,
such as "Is a high protein diet right for me?" or "Are eggs bad for my
health?" If they default to outdated wisdom without batting an eyelash,
then you may want to seek nutritional guidance elsewhere. - Pay close attention to whether or not their advice is specific and actionable.
Are their recommendations vague, such as "eat healthy" and "do things
in moderation?" or do they go into specific recommendations, such as
"keep a food journal and track calories." - Look at other credentials other than the "Dr." in front of their name. You can use this handy PDF
to search for a physician's certifications by any state. Are they
trained by the American Board of Obesity Medicine, the American Board of
Physician Nutrition Specialists, or something similar? - Be realistic about how well you get along with your doctor. Knowledge isn't everything. Your doctor can be the most knowledgeable in the world, but their advice can backfire if you feel that they are overly judgmental or lack empathy.
the resources you need in order to get (or stay) healthy and fit. Stay
as informed as you can on the latest nutritional research. Don't expect
your doctor's knowledge about medicine to apply to other domains. After
all—like you—they are only human.
Images by LalithHerath (Shutterstock), murphy81 (Shutterstock), katherinarspb (Shutterstock), caliorg, Jeremy Wong, and Ilmicrofono Oggiono.
Why Your Doctor Might Not Be the Best Nutritional Resource
Monday, February 9, 2015
6 habits to improve healing after surgery

A successful surgery depends on a number of factors -- a few of them you can control.
(CNN)The winter is surgery season.
Peopleget into skiing accidents and need to replace knees, or they slip on
ice and need to fix a hip, or they just want to get ready for bikini
weather and schedule a nip here and an enlargement there.
Surgeons are particularly busy these days, but Dr. Jamal M. Bullocks, a surgeon from the Kelsey-Seybold Clinic in Houston, has advice if you do need surgery.
A successful surgery depends on a number of factors -- a few of them you can control.
Even
minor surgery may pose some risk that has long-term implications. So,
for those considering surgery, there are six habits you need to commit
to right now to help your body heal.
Here's how Bullocks suggests you can improve your chances of recovering more quickly if you do go under the knife:
Quit smoking
Ishouldn't even have to tell you this. If you smoke, you know this habit
can cause irreparable damage to your organs. It increases your chances
for heart attack and stroke.
Smoking can significantly hamper
the success of your procedure. While in surgery, the damage from smoking
to your airway and lungs makes it more difficult to control your
breathing while you are under anesthesia.
Additionally, because
smoking damages your vascular system, it can bring on complications in
wound healing that may lead to infection and wound breakdown.
If
you smoke and have plans to go under the knife, talk to your physician
about smoking-cessation programs and products and follow his or her
advice.
Use this surgery as an opportunity to improve your overall health by quitting smoking.
Improve your diet
Malnutrition and the effects of poor eating habits can negatively alter how your body reacts to surgery.Malnutrition
is a serious condition that can affect overall health and is a concern
for many older adults since senior citizens are at particular risk.
Malnutrition
can weaken your immune system, cause muscle weakness that can decrease
cardiac and respiratory function and may negatively affect wound
healing.
Talk to your physician about your eating habits, and if
he or she determines you need help improving your diet, work with a
registered dietitian before surgery.
Consider supplements
Evenif you eat a well-balanced diet, your diet may still be lacking in
important vitamins and protein that promote healing after surgery.
Supplemental
vitamins (such as vitamins A, E and C) and protein can promote acute
wound healing -- and despite looking and feeling healthy, your body may
need a boost.
Ask your physician to confirm that you are not
deficient in any vitamins and to test your protein building capacity and
work with him or her to determine an appropriate supplement regimen
before surgery.
Manage your weight
This is easier said than done.Being
overweight or obese raises your risk because many people with this
condition have other risk factors such as cardiovascular disease,
respiratory abnormalities, heart failure, hypertension, pulmonary
embolism and deep vein thrombosis.
If you are overweight or obese
and considering a nonurgent surgery, work with your physician to develop
a weight-loss plan and try to attain a healthier weight.
It may help improve your overall condition as well as lower your surgery risk.
Manage chronic conditions
Diabetes,kidney disease and hypertension are just a few examples of chronic
conditions that may increase the chances of complications during and
after surgery.
It is important to be in the best possible condition before undergoing surgery.
If
you have a chronic condition that is not well-controlled, work with
your care team to help improve your outcomes before an elective surgery.
Follow your doctor's orders
You've chosen your surgeonto guide you through this experience based on a lot of things. You did
research on this procedure, and he or she came highly recommended. Such a
surgeon may have special credentials or certifications that make you
feel more confident.
You trusted your surgeon enough to start
down the path of preparing for this surgery, so why won't you listen
when we give you special instructions to follow beforehand?
Surgeons
are like every other kind of doctor; they want to help patients improve
their health, but they also want to minimize the risk of a condition
worsening as a result of the surgery.
This is a team effort, and
it is imperative you do your part to eliminate potential problems and
help with a successful outcome.
Follow your surgeon's instructions before surgery -- and always ask questions if something is confusing or unclear.
Subscribe to:
Posts (Atom)
